Krainc Lab Research
Parkinson’s disease: Examination of converging pathogenic pathways to identify key targets for therapeutic development
Parkinson’s disease (PD) is the second most common neurodegenerative disorder, characterized by progressive degeneration of SNc dopaminergic neurons leading to clinical parkinsonian symptoms (bradykinesia, resting tremors, muscular rigidity, and postural instability). Although the majority of patients do not have a family history of PD (sporadic PD patients), genetic studies have identified several genes which cause familial forms of PD including α-synuclein, LRRK2, VPS35, ATP13A2, PINK1, parkin, DJ-1 and GBA1. Furthermore, brains of sporadic and familial PD patients also show formation of Lewy bodies consisting of α-synuclein deposits, suggesting that α-synuclein accumulation and toxicity is a key player in PD pathogenesis. Our lab studies the function of multiple PD genes and converging cellular mechanisms both upstream and downstream of α-synuclein toxicity in order to ultimately identify new therapeutic targets for PD.
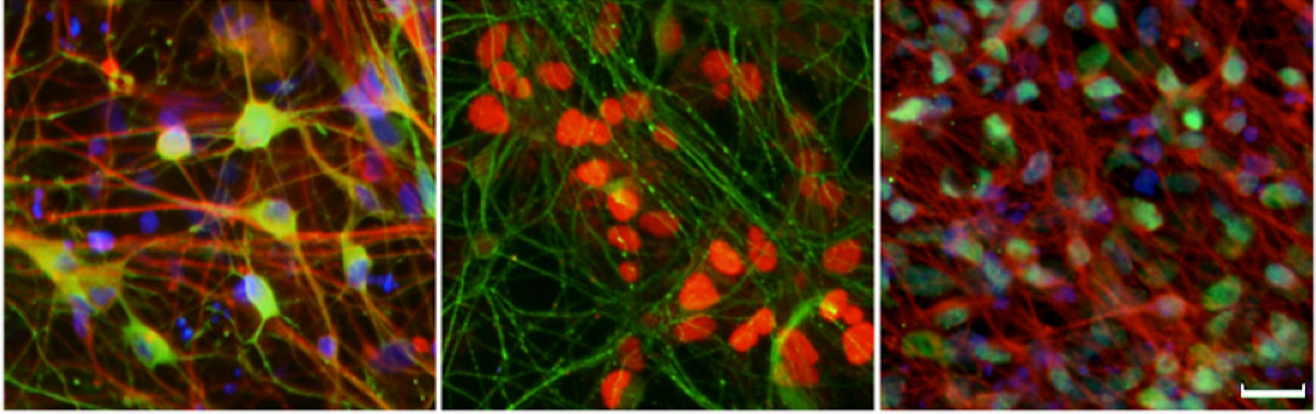
Using patient-derived induced pluripotent stem cells (iPSCs) differentiated into dopaminergic neurons, we have found that:
- Upstream dysfunction in multiple PD genes including ATP13A2, parkin, DJ-1 and GBA1 leads to α-synuclein accumulation and defects in both endolysosomal and mitochondrial pathways
- Downstream α-synuclein accumulation additionally results in lysosomal dysfunction by disrupting trafficking of multiple lysosomal enzymes including GBA1.
Key Papers
- LRRK2 phosphorylation of auxilin mediates synaptic defects in dopaminergic neurons from patients with Parkinson's disease. Nguyen M, Krainc D. Proc Natl Acad Sci U S A. (2018)
- Mitochondria-lysosome contacts regulate mitochondrial fission via RAB7 GTP hydrolysis. Wong YC, Ysselstein D, Krainc D. Nature. (2018)
- Analysis of blood-based gene expression in idiopathic Parkinson disease. Shamir R, Klein C, Amar D, Vollstedt EJ, Bonin M, Usenovic M, Wong YC, Maver A, Poths S, Safer H, Corvol JC, Lesage S, Lavi O, Deuschl G, Kuhlenbaeumer G, Pawlack H, Ulitsky I, Kasten M, Riess O, Brice A, Peterlin B, Krainc D. Neurology. (2017)
- Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson's disease. Burbulla LF, Song P, Mazzulli JR, Zampese E, Wong YC, Jeon S, Santos DP, Blanz J, Obermaier CD, Strojny C, Savas JN, Kiskinis E, Zhuang X, Krüger R, Surmeier DJ, Krainc D. Science. (2017)
- α-synuclein toxicity in neurodegeneration: mechanism and therapeutic strategies. Wong YC, Krainc D. Nat Med. (2017)
- Parkin Modulates Endosomal Organization and Function of the Endo-Lysosomal Pathway. Song P, Trajkovic K, Tsunemi T, Krainc D. J Neurosci (2016)
- α-Synuclein-induced lysosomal dysfunction occurs through disruptions in protein trafficking in human midbrain synucleinopathy models. Mazzulli JR, Zunke F, Isacson O, Studer L, Krainc D. Proc Natl Acad Sci U S A (2016)
- ATP13A2/PARK9 regulates secretion of exosomes and α-synuclein. Tsunemi T, Hamada K, Krainc D. J Neurosci (2014)
- Zn²⁺ dyshomeostasis caused by loss of ATP13A2/PARK9 leads to lysosomal dysfunction and alpha-synuclein accumulation. Tsunemi T, Krainc D. Hum Mol Genet (2014)
- Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Mazzulli JR, Xu YH, Sun Y, Knight AL, McLean PJ, Caldwell GA, Sidransky E, Grabowski GA, Krainc D. Cell (2011)
Personalized medicine: Targeting GBA1 in Parkinson’s disease
Our lab is ultimately interested in using patient-specific approaches to target neurodegenerative diseases including Parkinson’s, Huntington’s and Frontotemporal dementia (FTD). To accomplish this, we:
- Obtain patient-derived induced pluripotent stem cells (iPSCs) and differentiate them into neurons which we can grow and analyze in long-term cultures. We additionally use genetic sequencing and CRISPR-CAS gene editing technologies to help identify cellular pathways that are disrupted in these neurons.
- Use medicinal chemistry to identify small molecule drugs/compounds which can ameliorate these defects and test their efficacy in both cell and animal models.
- Bring these compounds we have identified back into the clinic to treat patients with these diseases.
Using patient samples, we have identified an important bidirectional loop between loss of GBA1 function (which causes Gaucher’s disease) and α-synuclein toxicity in Parkinson’s disease. Importantly, we have found that increasing enzymatic activity of the GBA1 protein (β-glucocerebrosidase) reduces α-synuclein accumulation and associated downstream toxicity in human neurons, and are now identifying novel compounds which efficiently target and activate GBA1 in order to reduce α-synuclein toxicity in Parkinson’s disease and other synucleinopathies.
Key Papers
- Conversion of Quinazoline Modulators from Inhibitors to Activators of β-Glucocerebrosidase. Zheng J, Jeon S, Jiang W, Burbulla LF, Ysselstein D, Oevel K, Krainc D, Silverman RB. J Med Chem. (2019)
- β-Glucocerebrosidase Modulators Promote Dimerization of β-Glucocerebrosidase and Reveal an Allosteric Binding Site. Zheng J, Chen L, Skinner OS, Ysselstein D, Remis J, Lansbury P, Skerlj R, Mrosek M, Heunisch U, Krapp S, Charrow J, Schwake M, Kelleher NL, Silverman RB, Krainc D. J Am Chem Soc. (2018)
- Acid ceramidase inhibition ameliorates α-synuclein accumulation upon loss of GBA1 function. Kim MJ, Jeon S, Burbulla LF, Krainc D. Hum Mol Genet. (2018)
- Design and Synthesis of Potent Quinazolines as Selective β-Glucocerebrosidase Modulators. Zheng J, Chen L, Schwake M, Silverman RB, Krainc D. J Med Chem (2016)
- Activation of β-Glucocerebrosidase Reduces Pathological α-Synuclein and Restores Lysosomal Function in Parkinson's Patient Midbrain Neurons. Mazzulli JR, Zunke F, Tsunemi T, Toker NJ, Jeon S, Burbulla LF, Patnaik S, Sidransky E, Marugan JJ, Sue CM, Krainc D. J Neurosci (2016)
- Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Mazzulli JR, Xu YH, Sun Y, Knight AL, McLean PJ, Caldwell GA, Sidransky E, Grabowski GA, Krainc D. Cell (2011)
Huntington’s disease: Gene transcription and degradation pathways
Huntington’s disease (HD) is a devastating genetic neurodegenerative disorder caused by polyglutamine (polyQ) expansions in the huntingtin protein, leading to striatal loss and clinical symptoms including chorea. However, the mechanisms through which mutant huntingtin leads to HD are still not completely understood.
We have found that
- Mutant huntingtin disrupts cellular transcription pathways which may contribute to neuronal death. Both soluble and non-aggregated mutant huntingtin interfere with transcriptional machinery to repress expression of target genes such as PGC-1α, a master regulator of mitochondrial function. In addition, the NAD-dependent deacetylase Sirt1 plays a neuroprotective role in HD models via its effects on TORC1, a brain-specific modulator of CREB transcriptional activity
- Modification of mutant huntingtin by acetylation leads to more efficient degradation of the mutant protein by autophagic/lysosomal degradation pathways. Based on these findings, we are currently identifying novel therapeutic agents which promote acetylation and degradation of mutant huntingtin to potentially prevent cellular death in HD neurons.
Key Papers
- Mutant Huntingtin Is Secreted via a Late Endosomal/Lysosomal Unconventional Secretory Pathway. Trajkovic K, Jeong H, Krainc D. J Neurosci. (2017)
- Sirt1 mediates neuroprotection from mutant huntingtin by activation of the TORC1 and CREB transcriptional pathway. Jeong H, Cohen DE, Cui L, Supinski A, Savas JN, Mazzulli JR, Yates JR 3rd, Bordone L, Guarente L, Krainc D. Nat Med (2011)
- Acetylation targets mutant huntingtin to autophagosomes for degradation. Jeong H, Then F, Melia TJ Jr, Mazzulli JR, Cui L, Savas JN, Voisine C, Paganetti P, Tanese N, Hart AC, Yamamoto A, Krainc D. Cell (2009)
- Transcriptional repression of PGC-1alpha by mutant huntingtin leads to mitochondrial dysfunction and neurodegeneration. Cui L, Jeong H, Borovecki F, Parkhurst CN, Tanese N, Krainc D. Cell (2006)
- In vitro analysis of huntingtin-mediated transcriptional repression reveals multiple transcription factor targets. Zhai W, Jeong H, Cui L, Krainc D, Tjian R. Cell (2005)
- Sp1 and TAFII130 transcriptional activity disrupted in early Huntington's disease. Dunah AW, Jeong H, Griffin A, Kim YM, Standaert DG, Hersch SM, Mouradian MM, Young AB, Tanese N, Krainc D. Science (2002)